
AHP Interactive
Case Study
A diagnostic journey of a patient with
acute hepatic porphyria (AHP).
Time: 3 to 5 minutes
This case is about a hypothetical patient.

Presentation - Severe, Diffuse Abdominal Pain
A Hypothetical Case of a Patient with Acute Hepatic Porphyria (AHP)
A 33-year-old female presents to the emergency room (ER) with severe, diffuse, abdominal pain that is burning in nature and associated with nausea and vomiting.
Attacks have occurred intermittently over 3 years and are now occurring every few months. they are sometimes associated with the patient's menstrual cycle.

DIAGNOSIS AND NEXT STEPS
Diagnosis:
Confirmed Acute Hepatic Porphyria
In this case, the ER physician referred the patient to a specialty clinic where they received a diagnosis.
Relevant Diagnostic Summary
- Multiple ER visits for episodes of severe abdominal pain
- Nausea/vomiting associated with episodes
- Constipation
- Numbness/tingling pain in back and legs related to abdominal pain
- “Brain fog” 2 to 3 days prior to episode
- Unremarkable physical exam
- Hyponatremia
- Elevated levels of ALA and PBG
Expert Insight
There is no typical presentation of AHP. 1,2,5
Although a characteristic symptom may lead to a diagnosis of AHP, no single sign or symptom is universal in every patient. Physical examinations typically show no abnormalities, and x-ray analyses appear normal or show mild ileus of the bowel in some cases. Some patients (<10%) may not even exhibit severe abdominal pain - the characteristic symptom of AHP.
Similarly, family history may be unrevealing because most carriers of the predisposing mutation in affected families are asymptomatic. Genetic testing can also be performed to help determine the patient's specific AHP type. The genetic test can also be used to help inform a diagnosis when a patient is not having an acute attack.
References
1. Anderson KE, Bloomer JR, Bonkovsky HL, et al. Ann Intern
Med. 2005;142(6):439-450.
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
5. Bissell DM, Anderson KE, Bonkovsky HL. N Engl J Med.
2017;377(9):862-872.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

DISEASE SPECIFIC TESTING
Could it be AHP?
Random (spot) urine testing for urine porphobilinogen (PBG) and urine delta-aminolevulinic acid (ALA) revealed high levels of PBG and ALA, and porphyrins.

A PBG random (spot) urine test can measure elevated levels of PBG. Substantial elevation of urinary PBG is a hallmark indicator of 3 types of AHP: AIP, VP, and HCP. ALA elevations can help confirm ADP—an extremely rare type of AHP. Urine porphyrins can help identify the type of AHP, but it is not recommended to use urine porphyrins alone as they can be elevated for several reasons.1,8
If AHP is suspected, consider ordering random (spot) urine tests to look for elevated levels of ALA and PBG, as well as porphryins.
*Normal ranges are based upon individual laboratory assay methodology.7rph
References
1. Anderson KE, Bloomer JR, Bonkovsky HL, et al. Ann Intern
Med. 2005;142(6):439-450.
7. Marsden JT, Rees DC. J Clin Pathol. 2014;67(1):60-65.
8. Bonkovsky HL, Bissell DM, Ventura P, et al. Poster
presented at: The Liver Meeting; November 9-13, 2018; San
Francisco, CA.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

LABORATORY RESULTS
AND IMAGING STUDIES
After an inconclusive physical examination, lab tests and imaging studies were ordered.
Laboratory Results
Urine pregnancy test: Negative
Additional lab work ordered
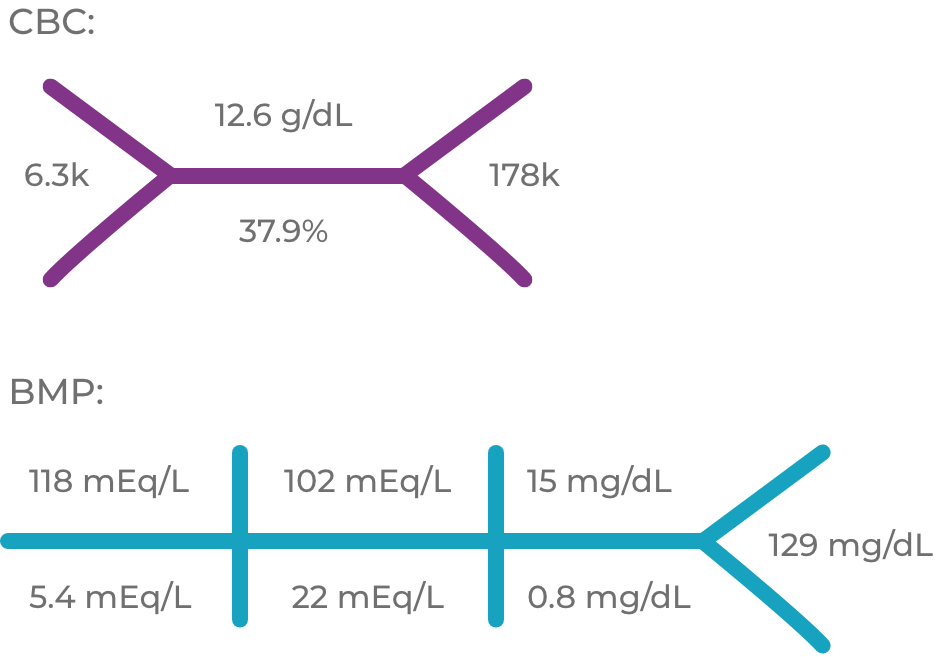
AST 19 U/L, ALT 27 U/L, amylase 77 U/L, lipase 30 U/L, alkaline phosphatase 97 U/L
ALT=alanine aminotransferase; AST=aspartate aminotransferase; BMP=basic metabolic panel; CBC=complete blood count
Full Lab Report

BUN=blood urea nitrogen; CK=creatine kinase; CPK=creatine phosphokinase; Cr=creatine; SGPT= serum glutamic pyruvic transaminase; SGOT= serum glutamic-oxaloacetic transaminase
Which lab value below might raise suspicion of AHP?
Imaging Studies
- Abdominal x-ray with normal bowel gas pattern
- Computed tomography of abdominal/pelvis with no evidence of abstraction or acute inflammatory process
Expert Insight
Hyponatremia is often observed during acute attacks. 2,5,6
Hyponatremia occurs in 25% to 60% of AHP cases when symptoms are present. When severe, it can lead to convulsions, which poses an additional therapeutic challenge, as many anticonvulsants are porphyrinogenic and may worsen an acute attack.
References
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
5. Bissell DM, Anderson KE, Bonkovsky HL. N Engl J Med.
2017;377(9):862-872.
6. Balwani M, Wang B, Anderson KE, et al; for the Porphyrias
Consortium of the Rare Diseases Clinical Research
Network. Hepatology. 2017;66(4):1314-1322.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

PHYSICAL EXAMINATION
The physical examination proved unremarkable except for mild tachycardia and hypertension.
Results of Physical Examination
- Vitals: T=98.5ºF, P=115, RR=18, BP=151/89, O2 sat=99% on room air
- HEENT: NCAT
- Cardiovascular: Regular rhythm, S1 S2, no murmurs, rubs, or gallops
- Lungs: CTA bilaterally
- Abdomen: Soft, mild tenderness, nondistended, +BS
- Skin: No rashes, no lesions, no erythema
- Musculoskeletal: No joint tenderness, redness
- Pelvic exam: No discharge, cervical motion tenderness, or adnexal tenderness
- Neurologic: Upper and lower extremities 5/5 proximally and distally, no cerebellar signs, no sensory deficit, normal lower
Expert Insight
AHP is often overlooked because the symptoms resemble those of more common conditions.3
When routine screening tests are negative, patients may be discharged with any of several less specific diagnoses, such as viral gastroenteritis, irritable bowel syndrome, psychosomatic pain, or addiction withdrawal.
BP=blood pressure; BS=bowel sounds; CTA=clear to auscultation; HEENT=head, eyes, ears, nose, and throat; NCAT=normocephalic, atraumatic; O2 sat=oxygen saturation; P=pulse; RR=respiratory rate; T=temperature.
References
3. Bissell DM, Wang B. J Clin Transl Hepatol. 2015;3(1):17-26.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

REVIEW OF SYSTEMS
Below are findings from a review of the patient's systems, which provided additional diagnostic clues
- Constitutional: No weight gain or loss; no fever
- Pulmonary: No shortness of breath
- Gastrointestinal: Occasional constipation; no bloody stool; no heartburn
- Genitourinary: No burning or pain with urination; no increased frequency
- Extremities: No clubbing, cyanosis, or edema
- Musculoskeletal: Numbness and tingling pain in back and legs related to abdominal episodes
- Neurologic: Difficulty concentrating (described as “brain fog”) 2 to 3 days prior to episode
Expert Insight
Prodromal symptoms of AHP2,4
Attacks typically begin with a prodromal phase, often including pain that is not abdominal and minor behavioral changes such as irritability, anxiety, restlessness, and insomnia.
In a 2016 study of patients with AHP who experienced acute attacks (N=16), all patients were able to identify prodromal symptoms at least 24 hours before an attack and, in most instances, recognized these symptoms 2 to 3 days before the onset of acute abdominal pain. One of the more frequently reported prodromal symptoms was “brain fog,” which patients described as a feeling of mental “cloudiness,” confusion, difficulty focusing, and disorientation.
References
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
4. Naik H, Stoecker M, Sanderson SC, Balwani M, Desnick RJ.
Mol Genet Metab. 2016;119(3):278-283.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

Patient Background and Medical History
Jane Doe
- 33 years old
- Caucasian
- Height 5' 7", weight 125 lbs
- Occupation: Unemployed
History of Present Illness
Chief complaint: Recurring episodes of severe, diffuse abdominal pain
- Multiple ER visits for episodes of severe, diffuse abdominal pain associated with nausea/vomiting
- Last ER visit was one month ago
—Treated with IV fluids and antiemetics - Pain is diffuse and severe
- Minimal improvement with narcotic pain medications
- Between episodes, moderate but tolerable level of abdominal pain
- Patient reports occasional constipation, no bloody stool
IV=intravenous
ER=emergency room
Should a suspicion of AHP be heightened based on the patient's gender?
Medical and Family History
Medical History
- Seasonal allergies
Medication
- Multivitamin
- Ciprofloxacin for uncomplicated urinary tract infection (completed one week prior to latest emergency room visit)
Family History
- Father died of myocardial infarction at 85 years of age
- Mother healthy
- No siblings
Expert Insight
Common clinical features of AHP1,2
AHP patients commonly present with severe, diffuse neurovisceral abdominal pain plus 1 or more additional symptoms:
- Nausea
- Vomiting
- Constipation
- Diarrhea
- Pain in back or thighs
- Tachycardia
- Hypertension
- Hyponatremia
- Dark, reddish urine
- Seizures (sometimes due to hyponatremia)
- Restlessness
- Hallucinations
- Other acute psychiatric symptoms
Physical examination shows no abnormalities, and x-ray analysis is normal or shows mild ileus of the bowel in some cases.
References
1. Anderson KE, Bloomer JR, Bonkovsky HL, et al. Ann Intern
Med. 2005;142(6):439-450.
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
3. Bissell DM, Wang B. J Clin Transl Hepatol. 2015;3(1):17-26.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

Correct Answer:
Sodium: 118 mEq/L. Hyponatremia occurs in 25% to 60% of AHP cases when symptoms are present. When severe, it can lead to convulsions.2,6
References
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
6. Balwani M, Wang B, Anderson KE, et al; for the Porphyrias
Consortium of the Rare Diseases Clinical Research
Network. Hepatology. 2017;66(4):1314-1322.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
05/20 AS1-USA-00011-V3

Correct Answer:
Sodium: 118 mEq/L. Hyponatremia occurs in 25% to 60% of AHP cases when symptoms are present. When severe, it can lead to convulsions.2,6
References
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
6. Balwani M, Wang B, Anderson KE, et al; for the Porphyrias
Consortium of the Rare Diseases Clinical Research
Network. Hepatology. 2017;66(4):1314-1322.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
05/20 AS1-USA-00011-V3

Correct Answer:
Sodium: 118 mEq/L. Hyponatremia occurs in 25% to 60% of AHP cases when symptoms are present. When severe, it can lead to convulsions.2,6
References
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
6. Balwani M, Wang B, Anderson KE, et al; for the Porphyrias
Consortium of the Rare Diseases Clinical Research
Network. Hepatology. 2017;66(4):1314-1322.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
05/20 AS1-USA-00011-V3

Correct Answer:
Sodium: 118 mEq/L. Hyponatremia occurs in 25% to 60% of AHP cases when symptoms are present. When severe, it can lead to convulsions.2,6
References
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
6. Balwani M, Wang B, Anderson KE, et al; for the Porphyrias
Consortium of the Rare Diseases Clinical Research
Network. Hepatology. 2017;66(4):1314-1322.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
05/20 AS1-USA-00011-V3

Correct Answer:
Occasional constipation, numbness and tingling pain in the back and legs related to abdominal episodes, and brain fog 2 to 3 days prior to an episode may all raise clinical suspicion of AHP.2,4
References
2.Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718): 924-937.
4.Naik H, Stoecker M, Sanderson SC, Balwani M, Desnick RJ. Mol Genet Metab. 2016;119(3):278-283.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
05/20 AS1-USA-00011-V3

Correct Answer: Yes
Correct Answer: Yes. Acute attacks are more common in women between the ages of 15 and 45. However, AHP can appear in men as well1,3
References
1. Anderson KE, Bloomer JR, Bonkovsky HL, et al. Ann Intern
Med. 2005;142(6):439-450.
2. Puy H, Gouya L, Deybach J-C. Lancet. 2010;375(9718):
924-937.
3. Bissell DM, Wang B. J Clin Transl Hepatol. 2015;3(1):17-26.
© 2022 Alnylam Pharmaceuticals, Inc. All rights reserved.
AS1-USA-00011-V3

SIGN UP TO RECEIVE UPDATES
About Acute Hepatic Porphyria From Alnylam
*All fields are required